Bag-Valve Mask
THIS PROCEDURE APPLIES TO: Any patient unable to adequately ventilate him/herself who needs supplemental oxygen delivered via a bag-valve mask.
EXCLUSION CRITERIA: None
PROCEDURE
- Observe body substance isolation precautions.
- Rescuer 1 should position him/herself at the top of the victim’s head. Rescuer 2 should kneel at the patient’s side.
- Open the patient’s airway and maintain it with an oropharyngeal airway.
- Because bag-valve masks are most effective when used by at least two rescuers working together, when two rescuers are available the bag-valve mask will be a two-person skill.
- When two persons use the bag-valve mask:
- Rescuer 1, using both hands, positions the mask to maintain a seal around the nose and mouth.
- Rescuer 2 squeezes the bag with both hands, delivering each breath over 2 seconds.
- Apply cricoid pressure throughout the entire procedure or until the patient is successfully intubated.
- If only one rescuer is available:
- With one hand, apply the mask to the patient’s face.
- Grip the mandible with the last two or three fingers while gripping the mask with the remaining fingers.
- Maintain head tilt and jaw lift while maintaining a seal around the nose and mouth.
- Compress the bag with the other hand while observing the chest to ensure chest rise.
- Connect the bag-valve mask to an oxygen source.
Ventilating the Conscious Patient
- To avoid resistance or combativeness due to fear, explain the procedure to the patient.
- Begin by matching the volume and rate of the patient’s ineffective breathing. Adjust the rate and volume until you are ventilating at the necessary rate and volume.
Ventilating During CPR
- Administer each ventilation over one second, regardless of the patient’s size or age.
- Each ventilation should be of sufficient volume to make the patient’s chest rise.
- Ventilations administered during CPR increase pressure in the chest. This pressure reduces the amount of blood that refills the heart and in turn reduces the blood flow generated by the next set of chest compressions. For these reasons, ventilating too frequently or with too large a volume (hyperventilating) may be harmful because it may reduce blood flow generated by chest compressions.
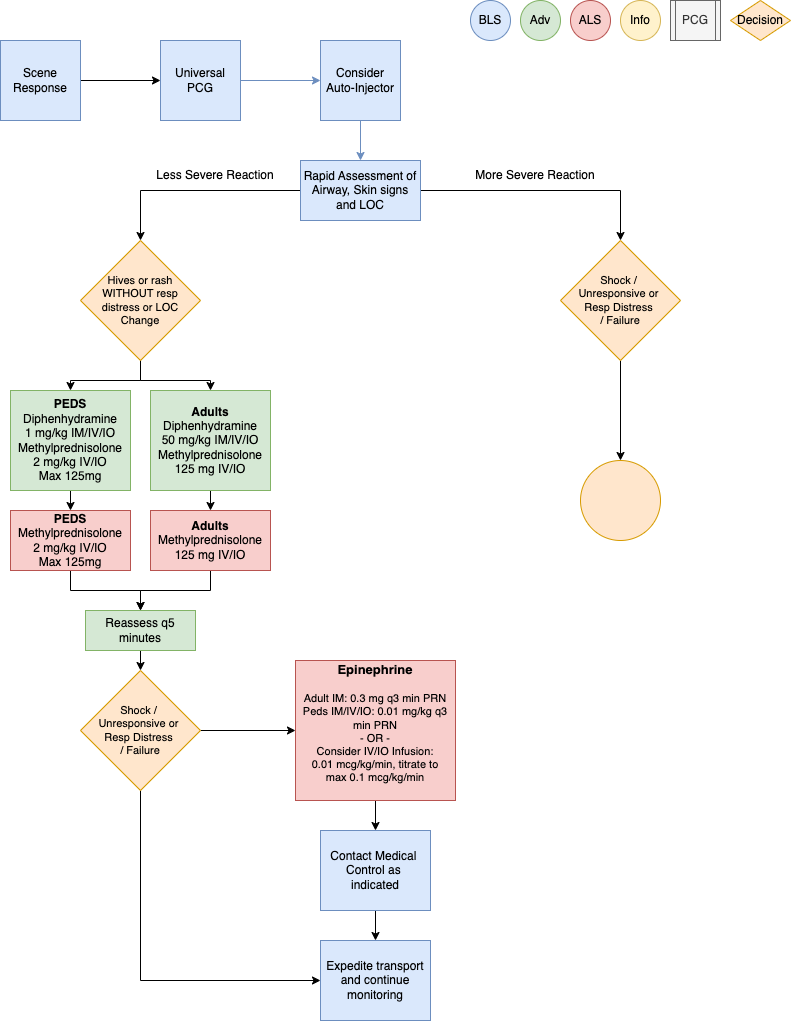
This policy applies to: Patients whose chief complaint is itching, rash or allergic reaction.
Exclusion Criteria: None
Recognize
- Itching, hives, flushing, angioedema
- Coughing, wheezing, stridor, or respiratory distress
- Chest or throat constriction
- Difficulty swallowing
- Difficulty phonating
- Nausea / vomiting
- Altered Mental Status
- Hypotension or shock
- Edema
Evaluate
- Onset and trajectory of symptoms
- Anatomic and situational location of exposure
- Insect sting or bite
- Known allergies: food, environmental, medication, other
- Known or suspected exposure: past occurrences and current event
- Known history of sensitivity or allergic reaction
- Past medical and medication history
- New clothing, soap, or detergent
- New medications
Administer Treatment
- Remove allergy trigger if known and present
- Prioritize interventions based on clinical presentation and severity of reaction
- Supplemental oxygen PRN for goal SpO2
- Attentive and prompt airway assessment and management
- Airway Management if indicated per Airway Management PCG (P1)
- If patient has suspected or known exposure and exhibits signs of any: respiratory distress, airway
restriction, altered mental status or shock, treat accordingly-
- Epinephrine Auto-Injector 0.3 mg IM if available
- Vascular access per Vascular Access PCG (P33)
- Consider crystalloid fluid bolus 500 mL IV/IO to support hemodynamics, repeat PRN
- Diphenhydramine (Benadryl) 50 mg IM/IV/IO
- Epinephrine (1mg/1mL) 0.3 mg IM or Epinephrine (1mg/10mL) 0.1 mg IV/IO q 3 min PRN for
MORE SEVERE REACTION-
- Consider Epinephrine infusion 0.01 mcg/kg/min IV/IO, titrate to max 0.1 mcg/kg/min
as an alternative to repeat IM or IV/IO doses - Monitor ECG rhythm closely, Epinephrine may potentiate arrhythmias, especially in
patients over the age of 40
- Consider Epinephrine infusion 0.01 mcg/kg/min IV/IO, titrate to max 0.1 mcg/kg/min
-
- Methylprednisolone (Solu-Medrol) 125 mg IV/IO
- Albuterol (2.5 mg/3 mL) nebulized for wheezing or shortness of breath
-
Consider Differentials
- Urticaria (rash only)
- Anaphylaxis (severe systemic effect)
- Shock (severe vascular effect)
- Angioedema (drug induced or infection)
- Aspiration / airway obstruction
- Vasovagal event
- Asthma or COPD
- Infection (ex: retropharyngeal abscess, bacterial tracheitis, croup, epiglottitis, strep)
- Pulmonary edema or CHF
- Metabolic disorders
Transport Considerations
- During transport, maintain astute airway, breathing, circulation and mental status assessment with
prompt intervention as needed. Stability can quickly change to instability in these patients. - Consider early airway management, reference Airway Management PCG (P1)
Information
- Typically, the shorter the interval from exposure to symptoms, the more severe the reaction
- Hemodynamic instability may recur up to 24 hours after initial stabilization
Other Populations
- Neonatal/ Pediatric drug dosing:
-
- Pediatric Epinephrine Auto-Injector JR dose is 0.15 mg for patients 15-30 Kg
- Diphenhydramine (Benadryl) 1 mg/Kg IM/IV/IO over 5 min max dose 50 mg
- Epinephrine (1mg/1mL) 0.01 mg/Kg IM/IV/IO q3 min until stable or infusion started
-
- Max 0.5 mg per dose (Intentionally larger than adult dosing)
- Epinephrine infusion 0.01 mcg/Kg/min IV/IO, titrate to max 1 mcg/kg/min
-
- Methylprednisolone (Solu-Medrol) 2 mg/Kg IV/IO max dose 125mg
- Albuterol for 15 Kg or more, use adult dose
- Albuterol for less than 15 Kg (1.25mg/ 3ml) nebulized with O2 at 6 lpm
-
Navigate
References
Campbell, Ronna. “Anaphylaxis: Emergency Treatment.” UpToDate, January 2022.
Sicherer, Scott. “Prescribing Epinephrine for Anaphylaxis Self-Treatment.” UpToDate, January 2022.
“U.S. Army Medevac Critical Care Flight Paramedic Standard Medical Operating Guidelines.” Jan. 2020.