Hypoglycemia - Maryland Format
Applies to: PatientsBlood glucose less than 70 mg/dL or greater than 300 mg/dL
- Patient-reported low or high blood glucose
- Diabetic patients with
bloodothersugarmedical<symptoms60(e.g.,mg/dlExclusion Criteria:NoneRecognize- vomiting)
- Altered mental status
AnxietyAlcohol intoxication, suspectedSlurred speechSeizureSweatingStroke symptomsPaleUnresponsiveskinpatientsTremorsCardiac SeizuresMedic alert bracelet / jewelryarrest
EvaluateBLS
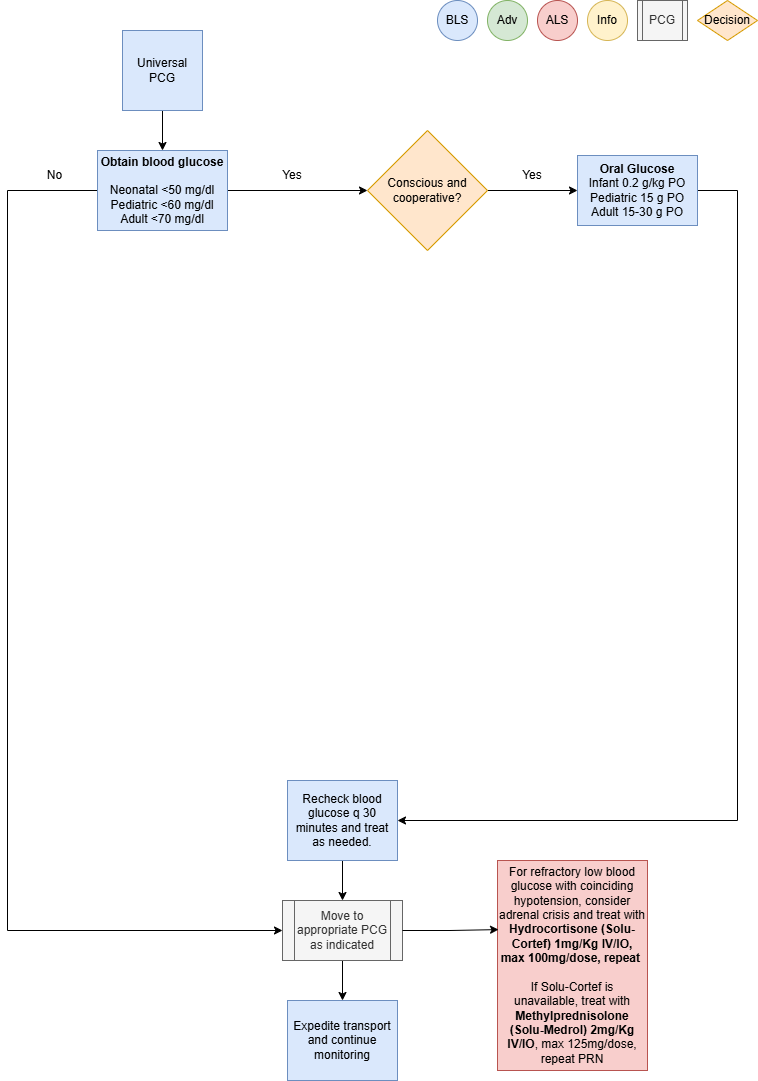
Primary survey with airway managementObtainCheck blood glucosemeasurementlevel- If blood glucose is less than 70 mg/dL, administer 10-15 grams of oral glucose between the patient’s gum and cheek.
- Administer additional dose of 10-15 grams of oral glucose if not improved after 10 minutes.
Administer TreatmentALS
- HYPOglycemia: If blood glucose is less than 70 mg/dL, administer 10% dextrose in 50 mL (5 gram) boluses, 1 minute apart, to a maximum of 250 mL OR 25 grams of 50% dextrose IVP, until:
- the patient has
altereda return to normal mentalstatusstatus,with concerns of inability to protect airway, obtain IV access,reference Vascular Access (P33)and Supplementaltheoxygen PRN for goal SpO2Adult: treat patients with apatient’s blood glucosereadingisofat<least7090 mg/dldLIf patient is conscious, cooperative and can protect their airway, administerOral Glucose 1-2tubes (15-30g) PO- If patient has persistently altered mental status
orandthereblood glucose less than 90 mg/dL despite treatment, repeat dosing regimen above. - If unable to initiate an IV and blood glucose is
concernlessofthaninability70tomg/dL,protect airway,
administerD10W,glucagon1251mLmg(12.5 gm) IV/IO over 10 minutes, may repeat PRN- IM/IN.
- If
D10Wtheispatient has persistently altered mental status and blood glucose less than 90
mg/dL at 15 minutes, transport to the hospital should notavailable,beadministerDextrose 50%, 25-50mL (12.5-25 gm) IV/IO over5 to 10 minutes, may repeat PRN
- If
- IM/IN.
ConsiderHYPERglycemia:Glucagon 1mg IM(>20 Kg patients) if venous access unobtainable
- the patient has
RepeatIf blood glucosemeasurementiseverygreater30thanminutes300andmg/dL,treatadministeraccordingly10 FormL/kgpersistentLactatedhypoglycemiaRinger’sdespitebolustreatment,unlessconsiderrales,awheezing,maintenancepedalinfusionedema,withorescalatingdextrosehistoryconcentrationof- renal
- failure
- or
D12.5%CHF isthe highest dextrose concentration that may be infused peripherallyDextrose concentrations higher than D12.5% require a central line or IO
- failure
For refractory low blood glucose with coinciding hypotension, consider adrenal crisis and treat withHydrocortisone (Solu-Cortef) 1mg/Kg IV/IO, max 100mg/dose, repeat PRNIf Solu-Cortef is unavailable, treat withMethylprednisolone (Solu-Medrol) 2mg/Kg IV/IO,max 125mg/dose, repeat PRN
Consider DifferentialsMC
EnvironmentalNotexposureToxic ingestionAlcoholismSepsisMetabolic etiologyAdrenal crisisApplicable
Transport Considerations
Blood glucose measurement is required on all patients less than 1 year of age, if not obtained atsending facility within the last 4 hoursHypoglycemia and hypothermia often coexist. If one of these conditions exists, determine if theother is also present
Information
Hypoglycemia should be considered in any person with an altered LOC. However, glucose should notbe administered unless the patient is actually hypoglycemic. Administration of glucose or dextrose toa patient who does not have hypoglycemia but instead has experienced a stroke resulting in analtered LOC could be detrimentalRemember that sick children have high metabolic requirements with high glucose utilization. Checkblood glucose early and oftenD10W is the preferred IV bolus solution to treat hypoglycemiaAbnormal glucose levels to be considered hypoglycemia and treated during transport:Adult < 70 mg/dlPediatric < 60 mg/dlNeonatal < 50 mg/dl
Other Populations
Neonate and Pediatric Dosing:Oral Glucose 0.2g/Kg PO(infant),15g POPediatricD10W, 2mL/Kg slow IV/UVC/IO over 10 minutes, may repeat PRNGlucagon 0.5 mg IM(<20 Kg) or1mg IM(>20 Kg) if venous access unobtainable
Neonate:Hypoglycemia has the potential for causing severe neurological damageSymptoms manifest mostly from CNS (jittery, high pitch cry, seizures)High glucose utilization may quickly deplete glycogen stores resulting in persistent hypoglycemiaConsider Inborn Error of Metabolism, specifically medium chain fatty acid deficiency (MCAD), in neonates with persistent hypoglycemia
Navigate
References
De Leon-Crutchlow, Diva D., et al. "Approach to Hypoglycemia in Infants and Children." UpToDate, Jul 2021.“U.S. Army Medevac Critical Care Flight Paramedic Standard Medical Operating Guidelines.” Jan 2020.Vella, A., et al. "Hypoglycemia in Adults without Diabetes Mellitus: Clinical Manifestations, Diagnosis, and Causes." UpToDate, Feb 2021.