Hypoglycemia
This policy applies to: Patients with blood sugar < 60 mg/dl
Exclusion Criteria: None
Recognize
Recognize
- Altered mental status
- Anxiety
- Slurred speech
- Sweating
- Pale skin
- Tremors
- Seizures
- Medic alert bracelet / jewelry
- Altered mental status
- Anxiety
- Slurred speech
- Sweating
- Pale skin
- Tremors
- Seizures
- Medic alert bracelet / jewelry
Evaluate
- Primary survey with airway management
- Obtain blood glucose measurement
Administer Treatment
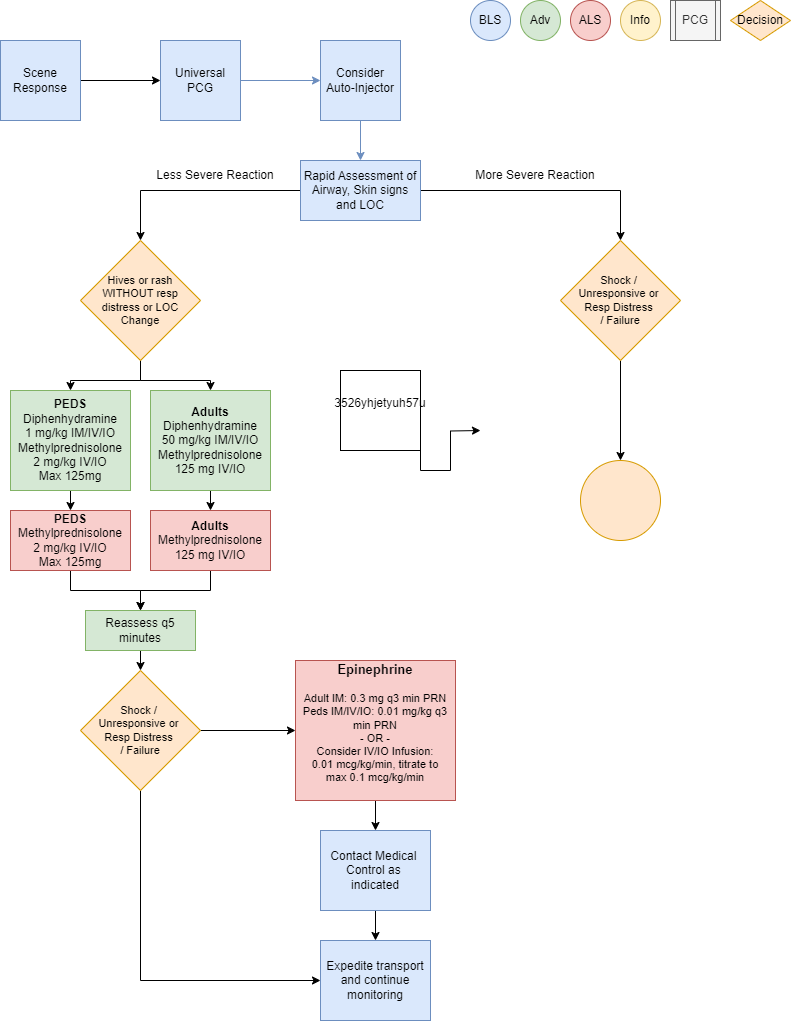
- Remove allergy trigger if known and present
- Prioritize interventions based on clinical presentation and severity of reaction
- Supplemental oxygen PRN for goal SpO2
- Attentive and prompt airway assessment and management
Airway Management if indicated per Airway Management PCG (P1) - If patient has suspected or known exposure and exhibits signs of any: respiratory distress, airway
restriction, altered mental status or shock, treat accordingly-
- Epinephrine Auto-Injector 0.3 mg IM if available
- Vascular access per Vascular Access PCG (P33)
- Consider crystalloid fluid bolus 500 mL IV/IO to support hemodynamics, repeat PRN
- Diphenhydramine (Benadryl) 50 mg IM/IV/IO
- Epinephrine (1mg/1mL) 0.3 mg IM or Epinephrine (1mg/10mL) 0.1 mg IV/IO q 3 min PRN for
MORE SEVERE REACTION-
- Consider Epinephrine infusion 0.01 mcg/kg/min IV/IO, titrate to max 0.1 mcg/kg/min
as an alternative to repeat IM or IV/IO doses - Monitor ECG rhythm closely, Epinephrine may potentiate arrhythmias, especially in
patients over the age of 40
- Consider Epinephrine infusion 0.01 mcg/kg/min IV/IO, titrate to max 0.1 mcg/kg/min
-
- Methylprednisolone (Solu-Medrol) 125 mg IV/IO
- Albuterol (2.5 mg/3 mL) nebulized for wheezing or shortness of breath
-
Consider Differentials
- Urticaria (rash only)
- Anaphylaxis (severe systemic effect)
- Shock (severe vascular effect)
- Angioedema (drug induced or infection)
- Aspiration / airway obstruction
- Vasovagal event
- Asthma or COPD
- Infection (ex: retropharyngeal abscess, bacterial tracheitis, croup, epiglottitis, strep)
- Pulmonary edema or CHF
- Metabolic disorders
Transport Considerations
- During transport, maintain astute airway, breathing, circulation and mental status assessment with
prompt intervention as needed. Stability can quickly change to instability in these patients. - Consider early airway management, reference Airway Management PCG (P1)
Information
- Typically, the shorter the interval from exposure to symptoms, the more severe the reaction
- Hemodynamic instability may recur up to 24 hours after initial stabilization
Other Populations
- Neonatal/ Pediatric drug dosing:
-
- Pediatric Epinephrine Auto-Injector JR dose is 0.15 mg for patients 15-30 Kg
- Diphenhydramine (Benadryl) 1 mg/Kg IM/IV/IO over 5 min max dose 50 mg
- Epinephrine (1mg/1mL) 0.01 mg/Kg IM/IV/IO q3 min until stable or infusion started
-
- Max 0.5 mg per dose (Intentionally larger than adult dosing)
- Epinephrine infusion 0.01 mcg/Kg/min IV/IO, titrate to max 1 mcg/kg/min
-
- Methylprednisolone (Solu-Medrol) 2 mg/Kg IV/IO max dose 125mg
- Albuterol for 15 Kg or more, use adult dose
- Albuterol for less than 15 Kg (1.25mg/ 3ml) nebulized with O2 at 6 lpm
-
Navigate
References
Campbell, Ronna. “Anaphylaxis: Emergency Treatment.” UpToDate, January 2022.
Sicherer, Scott. “Prescribing Epinephrine for Anaphylaxis Self-Treatment.” UpToDate, January 2022.
“U.S. Army Medevac Critical Care Flight Paramedic Standard Medical Operating Guidelines.” Jan. 2020.