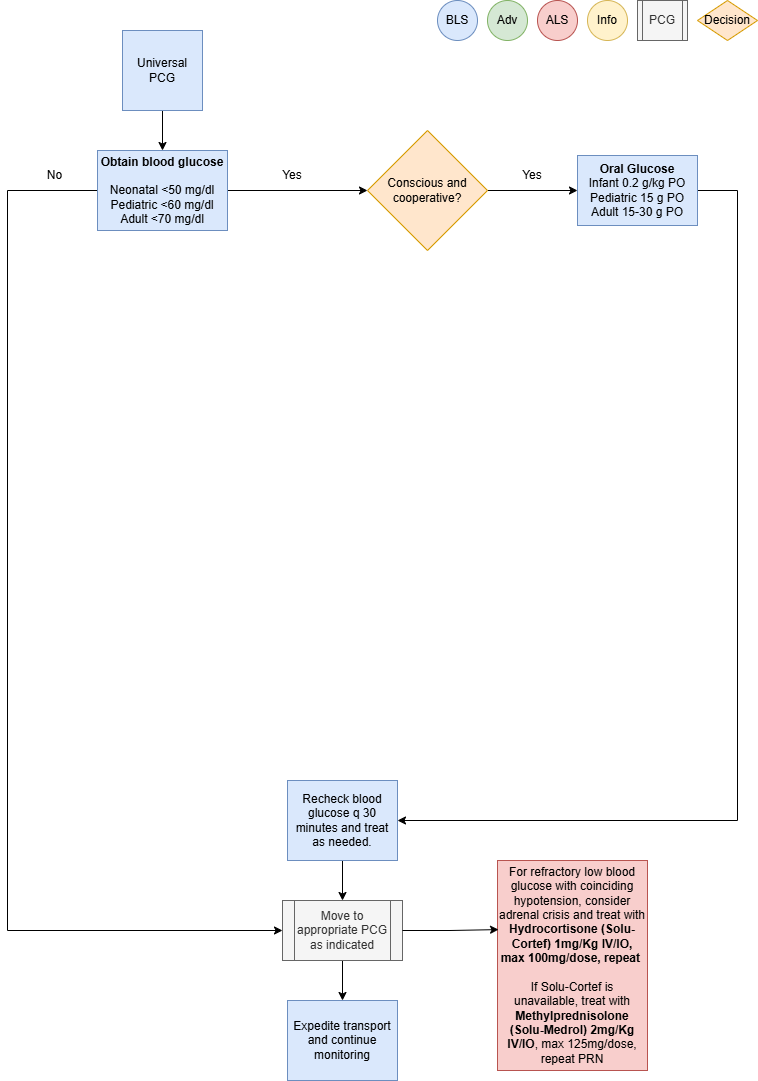
Hypoglycemia
This policy applies to: Patients with blood sugar < 60 mg/dl
Exclusion Criteria: None
Recognize
- Altered mental status
- Anxiety
- Slurred speech
- Sweating
- Pale skin
- Tremors
- Seizures
- Medic alert bracelet / jewelry
Evaluate
- Primary survey with airway management
- Obtain blood glucose measurement
Administer Treatment
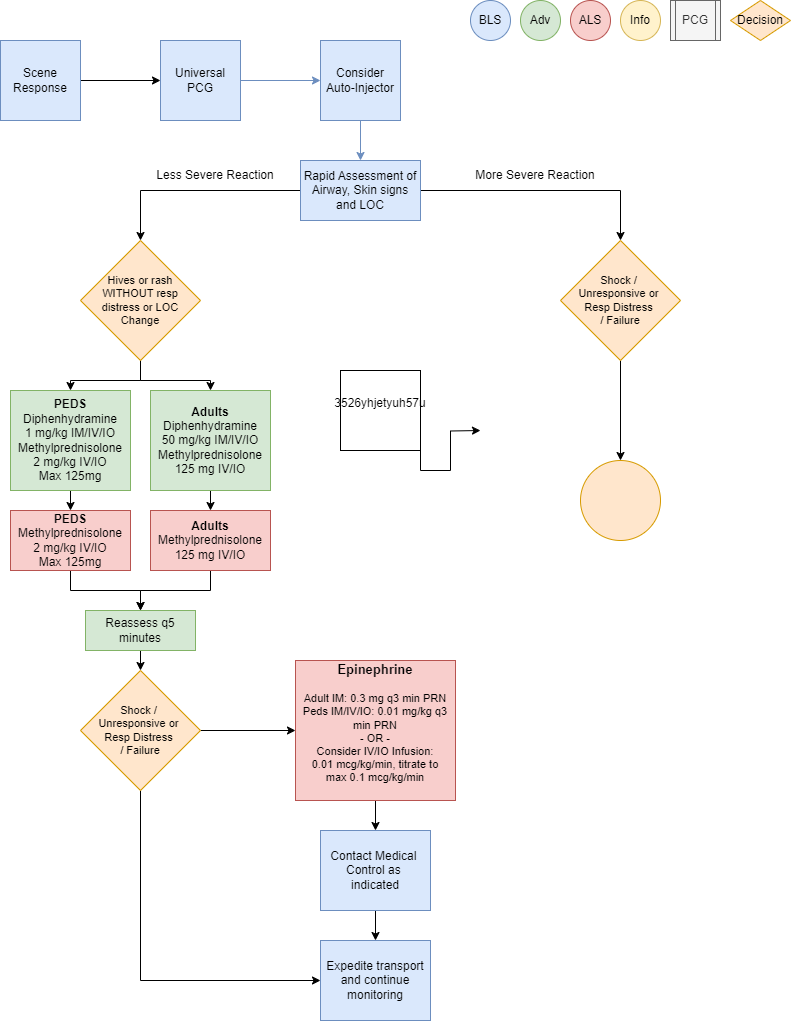
RemoveIfallergypatienttriggerhasifalteredknownmentalandstatuspresentwith Prioritize interventions based on clinical presentation and severityconcerns ofreactioninability to protect airway, obtain IV access,
reference Vascular Access (P33)- Supplemental oxygen PRN for goal SpO2
AttentiveAdult: treat patients with a blood glucose reading of < 70 mg/dl-
- If patient is conscious, cooperative and
promptcanairwayprotectassessmenttheirandairway,managementadminister Oral Glucose 1-2 Airway Management if indicated per Airway Management PCGtubes (P1)15-30g) PO - If patient has
suspected or known exposure and exhibits signs of any: respiratory distress, airwayrestriction,altered mental status orshock,theretreatisaccordinglyconcern of inability to protect airway,
administer D10W, 125 mL (12.5 gm) IV/IO over 10 minutes, may repeat PRN-
- If D10W is not available, administer
EpinephrineDextroseAuto-Injector50%,0.3 mg IMif available Vascular access per Vascular Access PCG25-50mL (P33)12.5-25 Considercrystalloid fluid bolus 500 mLgm) IV/IO over
5 tosupport10hemodynamics,minutes, may repeat PRNDiphenhydramine (Benadryl) 50 mg IM/IV/IOEpinephrine(1mg/1mL)0.3 mg IM or Epinephrine(1mg/10mL)0.1 mg IV/IOq 3 min PRN forMORE SEVERE REACTIONConsiderEpinephrine infusion 0.01 mcg/kg/min IV/IO, titrate to max 0.1 mcg/kg/minas an alternative to repeat IM or IV/IO dosesMonitor ECG rhythm closely, Epinephrine may potentiate arrhythmias, especially inpatients over the age of 40
- Consider Glucagon 1mg IM (>20 Kg patients) if venous access unobtainable
- If D10W is not available, administer
-
- Repeat blood glucose measurement every 30 minutes and treat accordingly
- For persistent hypoglycemia despite treatment, consider a maintenance infusion with escalating
dextrose concentration-
- D12.5% is the highest dextrose concentration that may be infused peripherally
- Dextrose concentrations higher than D12.5% require a central line or IO
-
- For refractory low blood glucose with coinciding hypotension, consider adrenal crisis and treat with
Hydrocortisone (Solu-Cortef) 1mg/Kg IV/IO, max 100mg/dose, repeat PRN-
- If Solu-Cortef is unavailable, treat with Methylprednisolone (Solu-Medrol)
125 mg2mg/Kg IV/IO , Albuterol125mg/dose,(2.5repeatmg/3 mL) nebulizedPRNfor wheezing or shortness of breath
max - If Solu-Cortef is unavailable, treat with Methylprednisolone (Solu-Medrol)
-
Consider Differentials
UrticariaEnvironmental(rash only)exposureAnaphylaxisToxic(severe systemic effect)ingestionShock (severe vascular effect)AlcoholismAngioedema (drug induced or infection)Aspiration / airway obstructionVasovagal eventAsthma or COPDInfection (ex: retropharyngeal abscess, bacterial tracheitis, croup, epiglottitis, strep)Pulmonary edema or CHFSepsis- Metabolic
disordersetiology - Adrenal crisis
Transport Considerations
DuringBloodtransport,glucosemaintainmeasurementastuteisairway,requiredbreathing,oncirculationall patients less than 1 year of age, if not obtained at
sending facility within the last 4 hours- Hypoglycemia and
mentalhypothermiastatusoftenassessmentcoexist.withpromptIfinterventiononeas needed. Stability can quickly change to instability inof thesepatients.conditions Considerexists,earlydetermineairwayifmanagement,the
otherreferenceisAirwayalsoManagement PCG (P1)present
Information
Typically,Hypoglycemia should be considered in any person with an altered LOC. However, glucose should not
be administered unless theshorterpatient is actually hypoglycemic. Administration of glucose or dextrose to
a patient who does not have hypoglycemia but instead has experienced a stroke resulting in an
altered LOC could be detrimental- Remember that sick children have high metabolic requirements with high glucose utilization. Check
blood glucose early and often - D10W is the
intervalpreferredfromIVexposurebolus solution tosymptoms,treatthe more severe the reactionhypoglycemia HemodynamicAbnormalinstabilityglucosemay recur uplevels to24behoursconsideredafterhypoglycemiainitialandstabilizationtreated during transport:-
- Adult < 70 mg/dl
- Pediatric < 60 mg/dl
- Neonatal < 50 mg/dl
-
Other Populations
- Neonate
Neonatal/and PediatricdrugDosing:dosing:-
PediatricOral Glucose 0.2g/Kg PO (infant),Epinephrine15gAuto-Injector JR dose is 0.15 mgPOfor patients 15-30 KgPediatricDiphenhydramineD10W,(Benadryl) 1 mg/2mL/KgIM/slow IV/UVC/IO over510minminutes,maxmaydoserepeat50PRNmgEpinephrine(1mg/1mL)0.01 mg/Kg IM/IV/IOq3 min until stable or infusion startedMaxGlucagon 0.5 mgper doseIM (Intentionally<20largerKg)thanoradult1mgdosing)IM Epinephrine(>20infusionKg)0.01ifmcg/Kg/minvenousIV/IO,accesstitrate to max 1 mcg/kg/minunobtainable
MethylprednisoloneNeonate:(Solu-Medrol) 2 mg/Kg IV/IOmax-
125mg- Hypoglycemia has the potential for causing severe neurological damage
AlbuterolSymptomsformanifest15mostlyKgfromorCNSmore,(jittery,usehighadultpitchdosecry, seizures)AlbuterolHighforglucoselessutilizationthanmay15quicklyKgdeplete glycogen stores resulting in persistent hypoglycemia- Consider Inborn Error of Metabolism, specifically medium chain fatty acid deficiency (
1.25mg/MCAD),3ml)innebulizedneonates withO2persistentat 6 lpmhypoglycemia
dose-
Navigate
References
Campbell,DeRonna.Leon-Crutchlow,“Anaphylaxis:DivaEmergencyD.,Treatment.”et al. "Approach to Hypoglycemia in Infants and Children." UpToDate,JanuaryJul2022.Sicherer, Scott. “Prescribing Epinephrine for Anaphylaxis Self-Treatment.” UpToDate, January 2022.2021.
“U.S. Army Medevac Critical Care Flight Paramedic Standard Medical Operating Guidelines.”Jan.Jan 2020.
Vella, A., et al. "Hypoglycemia in Adults without Diabetes Mellitus: Clinical Manifestations, Diagnosis, and
Causes." UpToDate, Feb 2021.
-
- If patient is conscious, cooperative and
-